Immunization schedule for infants, toddlers and young children
Are your child’s immunizations up to date?
It is important not to miss vaccine doses.
Vaccines help your child’s immune system produce its own antibodies to help protect him or her from specific diseases.
Following the routine schedule helps protect your child from specific diseases.
The CANImmunize app can help keep track of your child’s immunizations. It’s free and can be downloaded here:
Prevnar 13 Immunization Schedule for infants, toddlers and young children
Prevnar 13 may be given to infants as young as 6 weeks.
This 3-dose schedule (2+1) may be considered if Prevnar 13 is given as part of
a routine immunization program

- a Customary age for dose 1 is 2 months of age, but it can be given as young as 6 weeks of age.
- b Recommended dosing interval is 2 months.
- c Booster dose is recommended between 11 and 12 months of age.
For at risk infants, toddlers and young children, the recommended routine
schedule is a 4-dose schedule (3+1)
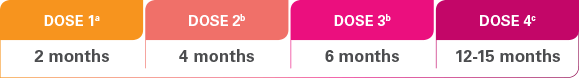
- a Dose 1 may be given as early as 6 weeks of age.
- b The recommended dosing interval is 4-8 weeks.
- c The fourth dose should be administered at approximately 12-15 months, at least 2 months after the third dose.
Prevnar 13 schedule for previously unvaccinated children ≥7 months
through 5 years of age
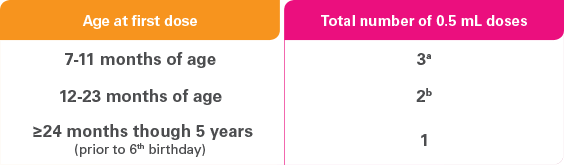
- a Two doses at least 4 weeks apart; third dose after the first birthday and separated from the second dose by at least 2 months.
- b Two doses at least 2 months apart.
Talk to your doctor, pharmacist or nurse about Prevnar 13 for your child.

FAST FACT:
Children who attend daycare (under 5 years old)
have been shown to be at increased risk of invasive pneumococcal disease (IPD).
What is invasive pneumococcal disease?

How does it work?
Vaccines teach our bodies to recognize and respond to viruses and bacteria, by making products called antibodies that help fight the disease. Our immune system can remember and fight them if they attack in the future.
The Prevnar 13 vaccine works by helping the body make its own antibodies, which helps protect you against diseases caused by 13 types of the bacteria Streptococcus pneumoniae.
Prevnar 13 safety information
Prevnar 13 should not be used if your child is allergic (hypersensitive) to the active substances, to any other ingredients, or to any other vaccine that contains diphtheria toxoid.
Take special care with Prevnar 13:
- If your child has any present or past medical problems after any dose of Prevnar 7 or Prevnar 13
- If your child is sick with a high fever
- If your child has any bleeding problems
Prevnar 13 will only protect against diseases caused by the types of Streptococcus pneumoniae covered by the vaccine. As with any vaccine, Prevnar 13 will not protect 100% of those who receive the vaccine.
Following vaccination with Prevnar 13, children and adolescents may experience redness, pain, tenderness (including impaired movement), swelling or hardness at the vaccination site, fever, irritability, drowsiness, restless sleep, decreased appetite, hives, diarrhea, vomiting and rash.
Talk to your doctor, pharmacist or nurse about vaccination with Prevnar 13.
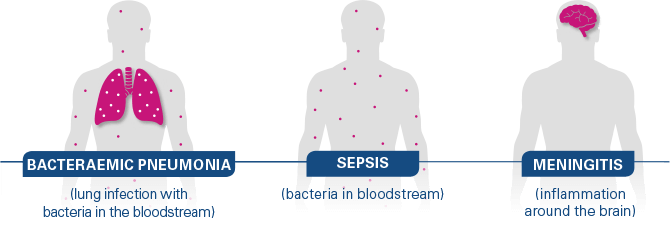
What is invasive pneumococcal disease (IPD)?
IPD occurs when bacteria called Streptococcus pneumoniae invades body sites that normally should not contain bacteria, such as the lining around the brain (meningitis), blood (sepsis), or lungs and blood (bacteraemic pneumonia).
IPD primarily affects:
- young children
- individuals with certain risk factors such as lifestyle or underlying medical conditions, and
- anyone 65 or over
In young children, bacteraemia accounts for 50 to 70% of all episodes of IPD, followed by pneumonia (15 to 25%) and meningitis (4%).
In adults, bacteraemic pneumonia accounts for 50 to 80% of all episodes of IPD.
“Invasive” disease means germs invade parts of the body that are normally germ-free.
Meningitis
Meningitis is inflammation of the covering of the brain and spinal cord and is generally caused by an infection.
Symptoms include:
- Stiff neck
- Fever and headache
- Pain when looking into bright lights
- Confusion
In babies, meningitis may cause poor eating and drinking, low alertness and vomiting.
COMPLICATIONS
Of children younger than 5 years old who get pneumococcal meningitis:
- About 1 out of 15 will die from the infection
- Others may have long-term problems, such as hearing loss or developmental delay
The chance of death increases among elderly patients.
Bacteraemia and sepsis
Bacteraemia and sepsis are infections where bacteria enter the bloodstream.
Symptoms include:
- Fever
- Chills
- Low alertness
COMPLICATIONS
About 1 out of 100 children younger than 5 years old with bacteraemia infection will die from it.
The chance of death is increased among elderly patients.
Bacteraemic pneumonia
Bacteraemic pneumonia is inflammation of one or both of the lungs with pneumococcus bacteria invading and entering the bloodstream.
Bacteraemic pneumonia accounts for 15-25% of the cases of IPD in young children and 50-80% of cases in adults.
- Fever and chills
- Cough
- Rapid breathing or difficulty breathing
- Chest pain
Older adults with pneumonia may experience confusion or low alertness, rather than the more common symptoms listed above.
COMPLICATIONS
- Infection of the space between membranes that surround the lungs and chest cavity (empyema)
- Inflammation of the sac surrounding the heart (pericarditis)
- Blockage of the airway that allows air into the lungs (endobronchial obstruction)
- - lung collapse (atelectasis)
- - collection of pus (abscess) in the lungs
Prevnar 13 is not indicated to reduce complications of IPD, including death, neurological complications or hearing loss.
How does it spread?

Can IPD be treated?
IPD can be treated with antibiotics.
Although Prevnar 13 can help protect against diseases such as meningitis, sepsis, bacteraemia and bacteraemic pneumonia caused by 13 serotypes of the bacteria Streptococcus pneumoniae, it is not intended to be used in the treatment of active infection.
As with any vaccine, Prevnar 13 will not protect 100% of those who receive the vaccine.